[Podcast] Bridging the Communication Gap Between Doctors and Patients

Fasiha Haq, Global Medical Education Advisor, Executive-Level Strategy and Execution, Eli Lilly and Company
I recently had the pleasure of speaking with Fasiha Haq, Global Medical Education Advisor at Eli Lilly and Company. This podcast is the fourth in a series of prep for our panel discussion at Eye for Pharma.
Lynn Nye, CEO of Medical Minds, co-moderated this podcast with me in advance of our panel discussion at this year’s EyeforPharma Conference in Philadelphia titled Patient-Centric Care: Does the Doctor Know Best?
To learn more about pharmaceutical marketing capabilities, see our sister company, Aria Agency, at AriaAgency.com.
“Focusing on patient experience”
Like other industry leaders, Ms. Haq believes the doctor-patient relationship has changed, “We are very much in the era of shared decision making and that looks different across cultures and diseases. “While doctors are certainly the experts in their field and have the skill and knowledge needed, Ms. Haq says, “Sometimes it's harder to see the bigger picture and recognize that although the patient is coming to you for medical care, holistically they are dealing with a lot of other things.”
She goes on to say asking a simple patient-centric question like ‘What’s top of mind for you?’ at the start of the visit can make all the difference in patient experience. Ms. Haq continues, “It tells [your patient] you’re listening and eager to provide care in a way that makes the most sense to them.” This is a terrific strategy to help bridge the communication gap we’ve been talking so much about.
Bridging the communication gap
Ms. Haq believes if you were to ask a patient and a doctor the same set of questions right after their visit together they’d have entirely different responses, “The physician may think he's done a great job of explaining options, explaining the disease and next steps, while the patient has heard something very different.” Ms. Faq says this is a big disconnect in the doctor-patient relationship.
Ms. Haq next shared a bit about Conversations in Motion, her four-module program that aims to realign the conversation between doctors and patients. So many, if not all, doctors have a limited amount of time to spend patients. As a result, we see doctors distilling a lot of information in a small amount of time. Ms. Haq believes that isn’t always the best strategy, “it’s very wise to pause and understand where the patient is coming from because then you have less of a discordance.”
Ms. Haq has seen success with her program as more and more doctors are taking a moment to ask patient things like, ‘What’s troubling you?’ or ‘Do you have any concerns we should talk about first?’ She says, “At the end of the day they say things like, ‘I just wish I could put my wedding ring back on,’ ‘Next week my son is getting married and I wish I could wear my heels’ or ‘I can't go to the mall, because of all the pain I'm in.’”
She further emphasized that following up with patient life events on their next office visit goes a long way in patient satisfaction, “Even if the patient expresses for 30 seconds how great they felt, the lasting effects in the neurotransmitters that are released in the brain have a very rich, restorative effect. It also positively affects how they see the disease—and their visit.”
Improving doctor involvement
Ms. Haq says the main goal for improving the patient experience in the pharma world is investing in improving people's health and lives, “we have to recognize that it goes much beyond just taking medication. There is a whole life to consider and only part of it is a treatment plan. To show that we, as a company, are committed to improving the patient's whole self and not just what benefits us, I think it's our important responsibility to help improve our patient’s lives holistically.”
Hi everyone. This is Stewart Gandolf with Healthcare Success and Aria Agency. I'm here today with Fasiha Haq who's in global medical education rheumatology at Eli Lilly. We're doing a panel together at this year's Eyeforpharma conference in Philadelphia along with Lynn Nye. Lynn's going to be actually moderating our discussion at the conference, so I thought it'd be fun to have her join us today's podcast as the moderator.
Fasiha Haq:
Stewart, I started with Lilly quite a number of years ago in Canada. I was actually in sales when I first started. After six years in sales, I actually joined the Canadian National Medical Education Team, so was working in the area of diabetes at the time, and at the time that I took the medical education role, it was because we implemented a program in sales in which we actually did exactly what you're saying in a sense on a much smaller scale of course, which was we put together physicians with other physicians versus patients. So what we did is we said "Okay, there's specialists who obviously know how to start patients on insulin. There are a group of physicians who want to learn how to start insulin, they're a little reluctant, but would like to take that next step" because we needed to ease that waiting list in the area, the geography that I represented, we needed to ease the waiting list for patients to be able to see an endocrinologist.
Fasiha Haq:
So we set up this mentorship program and that's when I moved into the Medical Education Team and we've rolled that out nationally because it was successful in a small geographical subset of Canada, but we were able to actually replicate it. And after spending, I would say a couple of years in the Canadian role, I moved into the global role, which is where I am now, so I have the privilege of working with multiple countries, so Asia, Pacific, Europe, obviously North America and South America as well. And my role now in the launch teams is all around developing the strategy with the medical affairs team and then distilling that into what does the medical objectives and then the global medical education objectives look like, and then bringing our regions sort of along with us on that journey of: a) how do you take a global strategy and localize it and what are the local considerations that we now need to take into account and maybe tweak that little strategy, and then how do we develop medical objectives out of that and how do we then develop a tactical plan which we can actually successfully execute. So it's been a lot of fun. And right now the area that I'm in is immunology and for the last few years really focusing on the rheumatology business.
Lynn Nye:
My first question to you is; you see when I started this I thought "Well the doctor does know that actually in lots of situations, but maybe they have difficulty keeping up with what's new." But then other people have very different views on this though, I'm going to ask you that question. What does to doctor know best and what are some of the things that doctors don't know, do you think?
Fasiha Haq:
It depends would be my answer, right? Yes and no. Certainly he is the expert that is looked at by a patient for the medical expertise, but how a patient wants to make that decision varies. We are very much in the era of shared decision making and that looks different across cultures and across types of diseases as well.
Fasiha Haq:
Some patients very much want to know everything. "So doctor, you know what, tell me all my options and make a recommendation." A second patient may walk in, they generally fall into three buckets. That's your first type of patient. In the era of Dr. Google, they may want to do their own searches and you know they want to understand all the options, but they do want to hear what the doctor has to recommend and then they'll think about it and come back. Then you have a second subset of patients who will say "You know doc, this is really overwhelming but you're the expert here. Just tell me what you think I should do." So there's that group of patients. And then there's a third group of patients who will say "Okay, you know, you've given me a lot of information but I need to, on my own, digest this, I need to think about some questions and I'm going to come back to you."
Fasiha Haq:
So everybody has their own way of dealing with things. And if you think about life in general, we're probably, with a little bit of deviance here or there, but we all kind of fall into these categories, right? So I think the doctor does know best when it comes to the medical expertise. Certainly that's where we rely on them. But what sometimes they get too focused on, and that's like all of us, when we know our area the best, we are very focused in on that piece. Sometimes it's harder to see the bigger picture and recognize that the patient, they're coming to you for this medical perspective, but holistically that patient is dealing with a lot of other things. And so, a) how does that patient like to receive information? Do I know this? If I know this as a physician, guess what? I can tailor my response accordingly.
Fasiha Haq:
So it's as simple as asking the question "How much information do you like to have before you make a decision?" And usually when I ask my patients, they say one of three things and it's usually one sentence, and I can share this with you in an email if you think it's useful. They say one of these three things, "which of these describes you best?" By doing that in a visit, you've just done a couple of things. You showed the patient, you matter, what you say matters to me, I'm listening to you, I want to do this in the way that makes the most sense to you. So already you're doing something to bridge that gap. And I think often, you know, we all are our human beings and we fall into this trap of when we're doing something we know well we fall into a habit. We the same thing the first time, the second time, the third time and the fourth time. But it is very wise to pause and understand where the patient is coming from because then you have less of a discordance.
Fasiha Haq:
The patient understands that you understand as a physician that you are concerned about their treatment goals, what are their motivations for making a certain treatment, how would you like to receive information, and that not only saves a physician time in the course of that one visit, it actually saves them time over time and it helps the patient to be on the same page. Because if you look at all the studies that are out there right now, what do they say? They show us that there is a great deal of discordance between patients and physicians when it comes to the understanding of what are their treatment goals and why they do what they do.
Fasiha Haq:
So I think there are very simple practices which often, not due to anyone's fault, it's just by our habit that we're in, can fall off the wayside. And even in the era of shared decision making, sometimes to some physicians that looks like just asking the patient which option do they think is best. But I think it's a little bit more than that and phrasing things a little bit differently, not only can it save them time, but it can also help to bridge that disconnect very, very quickly.
Lynn Nye:
And you started talking about what my next question was, this communication gap, this discordance between patients and physicians. But can you describe that a little bit maybe and give some examples?
Fasiha Haq:
I think I can share with you many references that we have come across, especially, which is why this conversation in motion, how this program came to be in fact. There are plenty of references and published papers now to show the discordance between patients and physicians. You can ask the patient questions after a certain visit and the physician the same questions and the physician thinks he's done a great job of explaining options, explaining the disease and next step. What the patient has heard is something very different. So the physicians will say "Well, I said it. Did you hear it?" Like did they hear what I said? No they didn't because the minute you told them that they have a chronic disease to which there is no cure, that patient has tuned out. They remember very little after that. So there is some time that's required for digesting and that's at the initial visit. "What happens, okay, now I know I have a chronic disease. There is no cure. We're on a treatment path."
Fasiha Haq:
But often physicians, not often, in fact, the majority of the time, what patients will tell you is "My doctor is focused on the long-term effects of this disease. And while I appreciate that I'm dealing with the short-term, which is today the pain, the fatigue or whatever the symptoms may be for that particular disease. And my doctor doesn't seem to care about that." It's not entirely true. The doctor does care. He is worried about the long-term. But his thought processes is that by giving them the appropriate treatment, not only will it help them in the long-term, but over time it will take care of the short-term symptoms except it will take a little bit of time, but they don't actually express that. The way it comes across to the patient is "Well, he keeps telling me, okay, my x-rays look normal, my MRI looks normal so I'm not worried about your joints. Let's just say if it was rheumatology could be any therapeutic area you choose and substitute the outcomes you're looking for.
Fasiha Haq:
But often when the patient goes in and says "Look doc, I am in so much pain, I have to wake up two hours early just to get ready in the morning." But the physician never addresses that directly. What they say is "Yeah, okay, I understand. So it's still bad, the pain is bad, but you know what? Here's what we're going to do. Your x-rays, all the results are looking good. Stick to this treatment or I'll make this slight change and you'll see a difference. Come back in six months." Six months is a long time, first of all. So what they take away from that visit is "He only cares about my joints. He's worried I don't end up in a wheelchair. I'm telling him I can't even get out of bed in the morning, but he never addressed that, right?" So that short-term versus long-term focus immediately creates discordance.
Fasiha Haq:
Asking a very simple question the minute they walk in and say "We've got 10 minutes for our visit today, what's top of mind for you?" If a physician said that to you the minute you walked in, guess what I feel immediately as a patient? This guy cares what I have to say. He wants to understand what is top of mind for me today, And you express that. And then the doctor could easily say "Great. So I hear you telling me that you're still in a lot of pain. Let's check your joints, let's do whatever needs to be done." And then always come back to that pain and say "Okay, you know what? Let's figure this piece out." But you've addressed it. By not addressing it that the patient feels you don't care or you're not interested in treating that symptom. They don't understand what is in the doctor's mind, which is "Hey, I'm changing this treatment and I know it will make an impact on both the signs and symptoms today and the long-term outcomes."
Fasiha Haq:
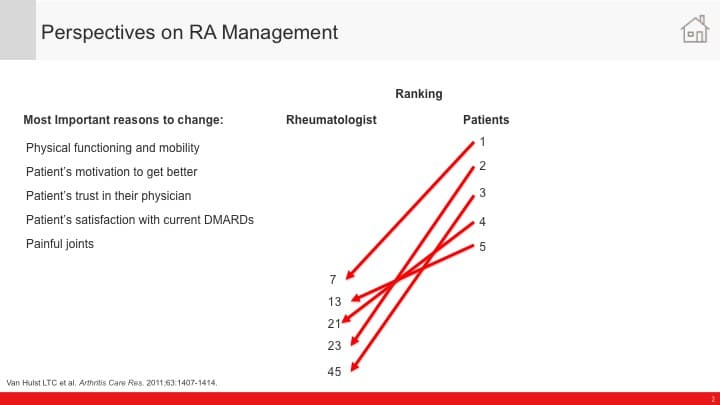
When you ask the patient's perspective of an HCP's role in in management of a disease, they say "You know, I wish my physician would tell me what the treatment goals are and how we are working towards them." The doctors are saying "I haven't done that." I can't believe that they're telling me that "I haven't done that." But what is creating that discordance, when you boil it down, it's simple issues and just addressing it straight forward with them. Because you know it's interesting when you take the top three things that patients are worried about and the top three things that physicians are worried about, they don't match up.
Fasiha Haq:
So the top things the physician is worried about is that the bottom of the patient's list and the top three things that the patient is worried about are at the bottom of the physician's list. And when you see it that way, like I'll send you the actual, not a graph, but I created this infographic because we talk about this all the time internally even when I'm trying to get funds for a particular project and show why this is important. But I created this infographic where it actually had arrows from what the patient's concerned and where it actually lands in the physician's mind and vice versa. And when people see that, it's like "Oh my God, no wonder we have a gap and disconnect if you will."
Stewart Gandolf:
We'd love to see that. And I think one thing that was very intriguing was, and this makes so much sense to me, is how the patient just stops listening, because when you get something that's bad news or on any patient gets bad news and they hear something that's "Oh my gosh, what does this mean?" The whole world sort of stops and goes into slow motion and the retention rate drops to, I don't know, you guys may have the numbers on this but I'm guessing around 10% tops. And the doctor may be talking very analytically about the disease and going through all the checklist, but the patient, we have to recognize the emotional component and that impacts our brain. So I don't know if you guys have any studies you guys have done on that or you can cite them but I think that's a really interesting point.
Fasiha Haq:
Yeah Stewart you know if you ever are interested or have time, I would love to show you the Conversations in Motion program because it is exactly that, and we've taken all of those points and distilled them into four modules. And the reason we did it that way was to be able to highlight some key things in a very, very, what shall we say, no nonsense way, talk about what are the communication gaps. I've got a 10 minute visit, how can I accomplish this in a 10 minute visit? And in that we actually have the four different types of patient. You'll have the patient who's learned that this information and it becomes very passive aggressive. And then one who is that yes patient. So how do you dive deep and find out what's in their mind and get them on that same page and what are the techniques that are utilized to actually do that? And it's as simple as one sentence in most cases and the effect however that it has, and we're just in the process of actually measuring this now to see how it can or cannot improve outcomes.
Fasiha Haq:
But that's exactly what that program tackles. And I can send you, like I said, a few bullets on each of these, but we have the videos to support what a... so we had a video recorded what a typical interaction between a physician and patient looks like and then what an interaction looks like utilizing the techniques that are in this program. And we timed it. And in fact it took less time when you employ the technique, because you're asking a targeted question and the patient is thinking about it and giving you a response. But the trust and empathy that it builds along the way actually is huge and it's very easy to do.
Fasiha Haq:
But sometimes it's as simple as we... it's again the habit, our default. Doctor walks in, he's looking through all the results, "Hey these look really good. You must be in really good shape." And so the patient immediately is like "Well, looks like all my test results are good. What's the point in me even speaking up about pain?" Half the time they don't even tell them. 55% of the time what they came in to say to the physician, they won't even address if the physician starts with "Hey, your test results look really good." And the majority of the time when the physician proactively asks a patient and says "So tell me, you know how you've been doing" studies show that within the first 18 seconds they're interrupted by the physician. So they've only had 18 seconds to express and in fact over, I think it's 90% of the time they never come back to that point. So then you can imagine why the patient walks away feeling like "You know what, it's all about what my doctor is..." and they don't feel that they're not doing a good job, they just feel like "You know what, it is what it is and I just have to live with the rest of the symptomatology and my doctor doesn't understand."
Lynn Nye:
Actually I think it might be because I've been talking with you so much, but my question is sticking with your mindset because my next question, what you just alluded to, is I think plays in communication, improves outcome and evidence, and what evidence is there just to prove this?
Fasiha Haq:
So what evidence is there to show that by improving communication we can actually improve outcomes?
Lynn Nye:
Yes.
Fasiha Haq:
There's definitely a lot of evidence. I'm trying to think of what will come top of mind for me, that is most recent in terms of evidence. But the Strand paper comes to my head right away because what it showed is that if in fact the patient feels that the doctor also has their motivation and their treatment goals in mind, that they are much more likely to be a) adherent to their treatment plan, and that doesn't just include medication, so that's why I call it a treatment plan because people think "Oh, it's just adherence to the drug." But what these studies have shown is that it results in more improved outcomes for the patient. So a) from a mindset perspective, they're much more positive and you know that that whole of self fulfilling prophecy, when we are positive about an outcome, we tend to behave and exhibit those types of thoughts and emotions that lead to a positive result.
Fasiha Haq:
So again, I'll be more than happy to send you this in an email to make sure I have it accurate, but in fact I will pull out the top few studies, more recent ones, to show that by employing the type of techniques that get patients to express their emotions and thoughts about how they're dealing with the disease, what their specific treatment goals are, what is it that they really want to do. When you ask a patient, let's say you have RA or any chronic disease, but you know "What is it really that to you?" At the end of the day they say things like "You know, I just wish I could put my wedding ring back on." "Next week my son is getting married, I wish I could wear my heels." "I hope to be a good role model for my kids because right now, my son or daughter has a practice and I can't even go, other moms can." "I can't go to the mall when my daughter wants me to go, because of all the pain that I'm in." So those are the basics for them, but the doctor never asks about these things.
Fasiha Haq:
And what studies show is that if they ask them what are their motivators and they record them in a chart and then they come back to them at the next visit and say "Hey, you know, you mentioned to me last time that you had wanted to wear those heels at the wedding. We gave you those cortisone shots. Did you wear the heels and how was that wedding?" Even if the patient expresses for 30 seconds how great they felt, the lasting effects in the neurotransmitters that are released in the brain actually have a very rich, not only restorative effect, but they actually have a very positive reinforcement within this patient's mind and how they see the disease, how they see the visit. When asked about the visit at the end "How long do you think your doctor spent with you? They'll say "Oh, I think he spent like 25 minutes." When in reality the doctor would likely just spent like 10 or 12 minutes the same as always, but they feel that it was much more because they ask them about "Hey, this was important to you. You mentioned it. Guess what? I heard it. It matters to me too. I wrote it down. I'm checking back in with you. How are you doing towards that? Now let's also focus on the long-term goals." Not saying it in that way, but "let's also focus on your test results, etc. etc."
Fasiha Haq:
But at the end of the day, I would say adherence and improved outcomes in their overall... how should I say an overall... how do I think I can cope with my disease? They answer in a much more positive manner. How do they end up coping with the disease and does it give them more incentive to do more? For example, they will end up trying things like exercise, like maybe cutting back on this or that, better sleep hygiene. They're much more open. So your mind actually, what they call the broaden and build theory. When your mind will be much more open to ideas and you will be much more likely to be more creative and productive and trying them if you are getting these positive reinforcements. There's a lot of data to show this.
Lynn Nye:
Yeah, thanks Fasiha. Actually it's interesting what you were saying because if you look in oncology for example there's so many studies these days that show that mindfulness, meditation has a positive effect on outcomes, right? Because when people are anxious, they don't want to continue with the therapies for a start. And secondly, anxiety really affects how the drug work, right?
Fasiha Haq:
Absolutely. In fact, I'm working on a big project right now around wellness. So we are developing actually a full module on understanding the science of wellbeing. In fact, I've just finished all of this research to show, now in 2019, there is so much more scientifically backed evidence around not just exercise, sleep and nutrition, which we've known for a long time, but mindfulness, meditation, random acts of kindness, even expressing gratitude and social connections. You will not believe the amount of evidence behind how much social isolation can be as big, if not more of a threat to longevity and overall long-term health as it's smoking or as other diseases. It's amazing what our minds have the ability to do and not do. So I agree with you. I mean that's just a whole other area where we're looking at holistic management now, and I expressed this idea of wellness and it's fascinating that in fact social rejection and isolation when they do FMRIs of the brain, the same regions light up as physical pain in your brain. So if somebody was beating you up basically, those same regions of pain that are lighting up in your brain are the same regions that light up for people who are lonely and socially isolated. Like, holy cow. So it's not just in your head, it's actually true.
Fasiha Haq:
And then the impact it has down the road in terms of your overall health and longevity, it's just mind boggling really. And these are all simple things but not so simple things, right? In the whole scheme of things.
Lynn Nye:
Well I think that's really important because one of the things that [inaudible 00:22:35] said to us is that our health care system today is really a sick care system. You go to the doctor when you're sick and the pendulum is really swinging to preventive care. In other words, wellness so that you don't get sick. And that's what our focus needs to be, especially in primary care. [crosstalk 00:23:03].
Fasiha Haq:
You're absolutely right because up until now it's always been a very disease-based mentality where, okay people are not well, how do we get them to neutral? And in the past 10 years, 15 years, the research is going the other way. This whole science of wellbeing is coming into play, because people are saying, "just because you're not ill does not mean you're well." So how do we get people north of neutral now? How do we move them from just being well where or just being okay or neutral or not ill, let's say, to wellness? so now that they've studied a whole bunch of that type of population and they've said "Okay, what's happening with that population and why haven't we studied that population? We're always studying the people who have illness or mental health issues but we're not studying the people that don't." And now that they've done that for many years and actually have produced scientific data behind it, those themes are the same.
Fasiha Haq:
Some of the things we've talked about, mindfulness meditation and the effect that it has on your prefrontal cortex, the reduction in anxiety, stress hormones, and even increasing the vagal tone. so there's all kinds of studies now to show why and how you can actually do it in our daily lives and why it should be important to you.
Stewart Gandolf:
Absolutely. I have a couple of questions that are stimulated by some of the comments I've just heard. The first question is, going back to the... I thought the social isolation was really compelling to me. What has your research shown, or do you have research out on how to help people with that? Because clearly the doctor, in many cases I'm assuming, you're close to this than me, it looks like that is beyond the scope of what they can help with. Is there any research or any ideas that you guys have for that? Because I could see how that would have a massive impact on overall wellness for almost any disease. What can you help us with on that?
Fasiha Haq:
So we have to be careful what we can say in our programs because anytime it comes from a pharma company, it becomes prescriptive and we can't be prescriptive. But I can tell you from my research, there are a number of great programs out there, Stewart. The Cleveland clinic has one. There's also one called The Wild Five. It's put out by Dr. Rakesh Jain, J-A-I-N, who is a psychiatrist and his wife is a wonderful lady, Saundra Jain, who is herself... I believe she is a nurse, a PhD and a psychotherapist. And they put out this wonderful workbook called The Wild Five, and what they've done is they've said "Okay, we are going to implement this in our clinic" and the reason I come back to that is because they actually have data to show the improved outcomes on these five things; exercise, nutrition, sleep and mindfulness and social connections or social connectedness is I believe how they term it.
Fasiha Haq:
And they actually give some ideas of what can you do. First of all, with all of their patients, they say to them "Okay, first of all, is this important to you? Is it important enough that you're going to stick to this program for 30 days?" And if the patient says yes, they say "What are you willing to give up to make it happen? Because every exercise may take five minutes or more, but you have to commit." And for those who do commit, it's been unbelievable in the outcomes that in terms of improving their rheumatoid arthritis in this case is what they focused on, and the pain associated with rheumatoid arthritis. Because again, pain is very subjective. It's in your mind and there's things you can do to actually impact what your perception of that pain is.
Fasiha Haq:
And what they prescribed and I'll say this in quotation marks in their workbook and what I've seen in others is very simple. Every day, give one person a call that you either you're close to or you have been close to, but you haven't touched base with them for a while. So whether it's every day or four times a week,. In fact, in most of my studies, this is what they show. They say either call someone and make a point of speaking to someone X times a times a week, or let's say if you're the type of person you don't have a huge family or a lot of friends or whatever, then make it a point to talk to someone in your day. If you're taking the subway, make sure to strike up a conversation. And they actually did these funny studies where people were taking the train and first thing in the morning, they said to half the people they met on the platform "Okay whoever you sit beside, I want you to strike up a conversation." And for the other half they said "Don't talk to anybody."
Fasiha Haq:
And they looked at their mood before and after, and they used a validated scale. And what they showed is that for the rest of the day, the people who did have a conversation with whoever was sitting beside them in fact were much more productive for the rest of the day, they were in much better spirits for the rest of the day, and that effect actually lasted for the week, believe it or not. And they made an effort to do it again. So again, that self-fulfilling prophecy. You see a gain, you want to do more of that behavior.
Fasiha Haq:
It's about making an effort or a conscious decision to have some sort of a social connection in whatever way fits your life. Whether it's giving somebody a call and talking to them. But it's not just about "Hey, how are you? I'm done." But also having a really substantiative conversation. So what they call high quality connections, HCQ. And that's really important because for those who have the high quality connections and meaningful conversation, that effect can actually be multiplied. So it's not to say your conversation with the Starbucks barista is useless because it's not. It will give you some amount of enhancement for the rest of the your day. But if you were to have a really meaningful conversation with someone at work or someone you're close to, that effect is in fact multiplied five fold. And that's sort of the cool thing about all this is it's not rocket science. It's not difficult to do, but it requires us putting in that effort to do it.
Stewart Gandolf:
The follow-up question to that would be; have you seen with these kinds of things, because certainly people, and I know people in family and elsewhere with like anxiety and depression, motivation isn't their strong suit oftentimes because it's overwhelming. Have you seen anything to help people to get motivation? Because I loved the fact that you ask them to buy in first, they have to commit. So what about the people who don't commit? Is there any help for that based upon what you've seen out there?
Fasiha Haq:
Yeah, actually there's a really, really good book by David Burns called Feeling Good, and in this book he shares how... so he talks about the cognitive behavioral therapy model that is now established and well utilized. But there are exercises in there that he actually applied with his patients with, deep depression, anxiety, no motivation, etc. And he employed actually several techniques and what he was able to show that without even any medication that these people in fact improved, ad it's ridiculous amounts. Like I even almost didn't believe it till I looked up some of these references, 60%, 50% in their mood.
Fasiha Haq:
So again, once they see a little bit of movement in the needle, it actually results in validating. "Oh my gosh, that really helped. Now I need to do this again." Or do they take more of an effort to do it? Is it easy? No. If the patient is just not there and it's like raising teenagers, right? If you tell them something and they just don't believe it or not willing to go there, no amount of motivation anyone has or you can give them will help. So yes, the patient does need to have a certain mindset of "I'm ready now and I'm willing to try something" because if they're not willing to try anything, then there's very little sometimes that you can do except for making sure that you're available and ready to meet them when they're ready to step up.
Fasiha Haq:
But there are very simple techniques. Like for example, mind chatter. What he says in there is just monitor your mind chatter. You know, we have like 60,000 thoughts a day and believe it or not, for the majority of the population, 80% of those thoughts are negative. You know, "I missed my meeting. God, I'm such an idiot. Why didn't I leave five minutes earlier? Here I go again." We're putting ourselves down. They say the way that we talk to ourselves, if we talked to other people that way you wouldn't have any friends, you've heard that quote before, and it's actually very true. So what he says in there is just start recording all your negative mind chatter for example. Every time you have a thought, replace it with a more digestible one. So you don't have to frame it as "Oh now let's just turn this into a happy happy thought and I'll be happy." No, it's turn this into a more realistic thought.
Fasiha Haq:
And he actually gives you some techniques that are so super simple. I actually tried a couple of these and it's really mind boggling that easily he was able to show in there that it improved outcomes in terms of reducing a patient's depression, anxiety, stress, and improving their mood in terms of the disorders using the DSM questionnaires that he uses over time if they were to be consistent with it. But your point well taken Stuart that, yes, it does require some level of agreement from the patient that "Yes, I want to try something."
Stewart Gandolf:
I have one final question. If I were to have talked to some of the doctors I work with at hospitals I work with on a daily basis who have a different viewpoint, they would probably ask "This is great. Why is pharma in general interested in patient experience?" Like what are the motivations because it's this is a new trend even with hospitals. Why do you think there's interest in this topic now and where do you see it going?
Fasiha Haq:
I think the main motivation for us in the pharma world is to step up and walk the talk, if you will. At the end of the day, what is our goal for developing new medication? It is about improving patient's life. So if we're truly invested in improving people's health and lives, we have to recognize that it goes much beyond just taking a pill, right? It's much more than just the medication. We as people are complex individuals. We have a holistic life, part of which is a treatment plan, but there are many other components of that life. And to show that we as a company are committed to improving the patient's whole self and not just what benefits us, I think it's very important and we have a responsibility to also invest in those types of initiatives that help patients improve their lives in all other domains as well, without being prescriptive of course, but making sure that we have through education and through things that we support, a) we show our commitment to those patients and to our physicians who treat those patients.
Fasiha Haq:
And we try and provide resources that can help in other domains of their life as well. But for me personally, I think that's the motivator to say I've worked for this company and I feel privileged to work in an industry where we have the opportunity to contribute to, whether it's treatment options, but much more holistically than that, contribute to creating resources that may help outcomes for patients, and help improve their lives in general, whether they have chronic disease or they don't, quite honestly, because I think we all struggle as human beings to say how can we improve ourselves in some domain or other and from a pharma standpoint, I think it's time to step up and do much more than just address that one aspect of a patient's life, which is focused around medication.
Lynn Nye:
I like that Lilly actually as it's a very different pharma company, actually. There are other pharma companies that are talking the talk about patient-centricity. Do you think it's widespread? I mean, is everybody doing it?
Fasiha Haq:
You know, I think people are definitely investing much more holistically than in the past. I think in the past it's been very much about "Okay, if we're in a particular area, for example, we focus on that one area."
Fasiha Haq:
I think companies are in different phases, if you will, but I think they're all recognizing that it's much more than just focusing on a specific area that you're working in. Because one of the biggest criticisms we've heard from our our physicians is that, you're all over us when you have a drug in that therapeutic area. The minute you don't have anything you walk away. And then five years down the road if you something else, you come back to us and you want us to be all in. We need to see much more of a commitment to that patient and to us, in this disease state, if you want our collaboration and if you say that you are as committed as you are to improving patient outcomes.
Fasiha Haq:
Because while you walked away for those five years, patients still had that disease. I was still a physician treating those patients. So what Lily's really trying to focus on, what is some of does things in our portfolio look like that can contribute to overall wellness, understanding things like the science of pain, etc. I think we're recognizing definitely that there's things we need to do that and we can do better. So I would say that I think every company is definitely exploring that possibility and trying to understand what is the best way that they can go about doing something like that, in a way that is appropriate for pharma. So I agree with you, I think we're all in different phases, but I do think that it is top of mind for people in the majority of the companies I've seen other types of communication kind of programs in the areas of dermatology, diabetes certainly. So there's much more of a willingness to invest, let's say, in these types of initiatives than there was, you know, let's say even 10 years ago or five years ago.
Lynn Nye:
So I guess the last question, and we're getting close to the hour here is about how to scale this? How to actually get physicians involved in doing this and how to spread the word and get commitment to it?
Fasiha Haq:
Yeah, and I think this is where we need better partnership, quite honestly. And sometimes it needs to be the physician that are driving it a little bit because I think there will always be some amount of skepticism when a pharma company is trying to drive something like this, and healthy often in the case because we've proven ourselves in the past to live up to that criticism unfortunately. So I think we do need some collaborative way where you have patient advocacy groups working hand in hand with physician groups and really driving in a much more unbiased way to say "Okay, if we believe in this then what are the kinds of programs that we are willing to have, for example, in our centers to drive this."
Fasiha Haq:
And we were seeing a lot of those, the Cleveland Clinic is an excellent example of a major institution who puts a lot of focus on wellness. If you look up some of their programs, they're really amazing. Every conference that they have incorporates those practices in the conference. So they're truly, you know, walking the talk now. And so I don't think it's something any one industry can do alone. It does require that buy in, and I think we're seeing more of it now that we have scientific evidence behind some of these strategies. And maybe it's about that peer-to-peer learning, right? So the things that are going well in some of these clinics, it's not just in the U.S., Europe, in the Danish countries and the Scandi countries, they are very, very advanced and truly believe in that whole wheel of life and addressing all the different domains, not just the health care domains. You can see that there's evidence and I think maybe bringing some of these learnings to the forefront and maybe pharma having a role, but maybe not leading that effort because again, I think that will bring it much more credibility than if it's just pharma bringing it to the forefront.
Fasiha Haq:
That was lovely to talk with all of you. Thank you so much for your time.
Stewart Gandolf:
Great. We enjoyed it as well. Thank you.